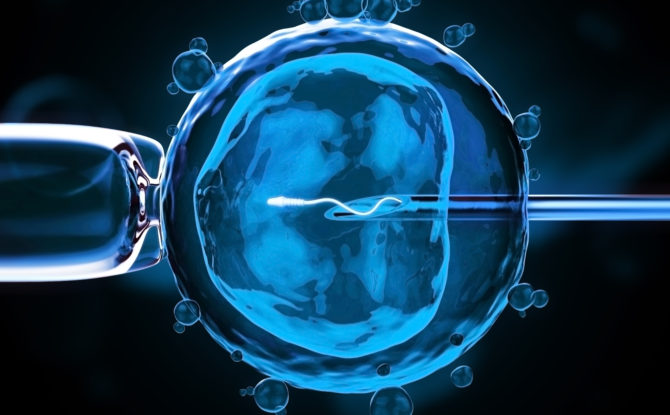
A few months ago, after a fertility procedure at a Mexican clinic, a healthy baby boy was born in New York to a couple from Jordan. It was the first live birth of a child who has been called — to the dismay of scientists who say the term is grossly misleading — a three-parent baby.
“This is huge,” said Dr. Richard J. Paulson, president-elect of the American Society for Reproductive Medicine, after the birth was reported on Tuesday of a three-parent baby.
The method used to help the couple is one that reproductive scientists have been itching to try, but it is enormously controversial because it uses genetic material from a donor in addition to that of the couple trying to conceive. The purpose is to overcome flaws in a parent’s mitochondria that can cause grave illnesses in babies.
Mitochondria, the cell’s energy factories, are separate from the DNA that determines a child’s inherited traits. But mutations in these little organelles can be devastating, resulting in fatal diseases involving the nerves, muscles, brain, heart, liver, skeletal muscles, kidney and the endocrine and respiratory systems that often kill babies in the first few years of life.
The technique that led to the healthy birth was to move the DNA from an egg of the mother, who had mutated mitochondria, and place it in the egg of a healthy egg donor — after first removing the healthy donor’s nuclear DNA from her egg cell. Then that egg, with its healthy mitochondria and the mother’s DNA, could be fertilized.
More than a decade ago — before controversy forced the work to stop — researchers tried a simpler technique that did not involve swapping nuclei between eggs. Instead, they injected some healthy mitochondria into an egg in an attempt to help with repeated failures at in vitro fertilization. It was not a method that could be used to prevent the birth of children with mitochondrial diseases.
The story of the Jordanian couple’s procedure began in 2011 when they came to see Dr. James Grifo, a professor of obstetrics and gynecology at New York University who pioneered the method in studies with mice. He referred them to his former student Dr. John Zhang, medical director of the New Hope Fertility Center in New York. Dr. Zhang had tried the method in 2003 in China, but the 30-year-old woman’s twins were born prematurely and died, though their mitochondria were normal.
When Dr. Zhang told the Jordanian couple about the technique, they hesitated. They already had a child who was terribly ill with Leigh syndrome, a mitochondrial disease, but there was a chance they could have a normal baby on their own — a quarter of the woman’s mitochondria were mutated, but mitochondria are distributed at random in eggs. If an egg with mostly good mitochondria happened to be fertilized, the baby would be fine. They decided to take their chances.
New York Times, by Gina Kolata – September 27, 2016
Click here to read the entire article.